Telehealth technology, including telehealthcare programs, has emerged as a crucial solution for providing healthcare services in remote areas. Telehealth visits are now a common practice in rural telehealth programs. With the advancements in technology, telemedicine offers an innovative way to bridge the gap between patients and healthcare providers, especially in rural communities. Telehealth services, telehealth programs, and telehealthcare programs have made it possible for patients to have virtual telehealth visits with their healthcare providers. Rural hospitals in remote communities often face significant challenges in accessing quality healthcare due to limited resources, geographical barriers, and disparities. However, telehealthcare programs can help bridge these gaps.
However, successful implementation of rural telehealth and telehealthcare programs in remote areas requires overcoming connectivity challenges. The lack of reliable broadband internet connection can hinder the use of asynchronous telemedicine, including remote patient monitoring, consultations with physicians, critical care support, and even pharmacy services. To ensure effective rural telehealth use in these regions, low-tech telehealth programs are being explored to address connectivity issues and provide accessible telehealthcare options for remote communities.
We will also explore the need to overcome connectivity obstacles for successful implementation of telehealth services and highlight some low-tech solutions that can help bridge this gap effectively in telehealth programs.
Impact of Telehealth on Rural Healthcare Access
Telehealth services, including telehealthcare programs and telemedicine use, have revolutionized access to specialized medical care for rural populations. These services, such as asynchronous telemedicine and remote consultations, have greatly improved healthcare accessibility. With the implementation of telehealthcare programs and technologies in remote areas, individuals residing in rural communities now have the opportunity to receive healthcare services, including pharmacy services, that were previously inaccessible to them. These telehealthcare programs also offer reimbursement for the services provided.
One of the key advantages of telehealth is the use of telemedicine technologies for remote healthcare services, resulting in reduced travel time and costs for patients. Additionally, telehealthcare offers potential reimbursement opportunities. In remote communities, where medical facilities are often located far away from residential areas, traveling long distances to health centers can be both time-consuming and expensive. However, with the advancement of telehealthcare, residents in these areas now have access to remote health care services. However, with telehealthcare programs in place, individuals from remote communities can have remote consultations with healthcare providers from the comfort of their own homes, eliminating the need for arduous journeys and allowing for remote presence.
Moreover, telehealthcare has enhanced the ability of person healthcare providers to provide timely medical interventions using virtual care technologies, leading to better health outcomes in remote areas. In situations where immediate medical attention is required, telehealthcare services using remote presence technologies allow healthcare professionals to swiftly assess patients’ conditions and provide necessary guidance or treatment. This prompt response from medical care providers can significantly impact health outcomes during the pandemic by preventing further deterioration and ensuring that appropriate measures are taken without delay through telehealthcare.
Rural populations in remote communities often face numerous health disparities and inequities due to limited access to healthcare resources. The pandemic has further highlighted the need for telehealth services to bridge the gap and provide remote communities with essential healthcare support. However, with the integration of telehealthcare technologies into rural healthcare systems, these barriers in remote communities are gradually being overcome, especially during the pandemic. Telemedicine, also known as telehealthcare, enables providers in remote communities to connect with specialists located in urban centers or academic institutions through virtual consultations, providing remote care through telehealth services. This collaboration ensures that patients in rural areas receive comprehensive telehealthcare and benefit from expert opinions through telehealth services, regardless of their geographical location.
Furthermore, the use of telehealthcare technologies has also led to an improvement in overall efficiency within remote communities, rural hospitals, and health centers. By utilizing telehealthcare technology for remote consultations and monitoring, healthcare professionals can optimize their workflow and allocate resources more effectively. Telehealth services are especially beneficial in rural areas where access to healthcare is limited. This streamlined approach not only benefits patients in remote communities but also enhances the capacity of rural healthcare facilities to deliver high-quality telehealth services.
Overcoming Connectivity Challenges in Remote Care
In rural areas, limited internet infrastructure and poor connectivity options pose significant challenges for telehealth services and virtual care consultations. However, it is crucial to identify alternative solutions to ensure reliable communication and access to telehealthcare services in these rural and underserved communities.
Limited Internet Infrastructure and Poor Connectivity Options
In rural areas, remote settings often lack the necessary internet infrastructure required for seamless telehealthcare services. This can be a challenge for healthcare providers looking to implement telehealthcare in these areas. The absence of high-speed internet connections and reliable networks hampers the delivery of telehealthcare, telehealth services, and remote monitoring devices in rural health. This limitation creates disparities in healthcare access for individuals residing in rural areas, where telehealth services and telehealthcare are limited.
Importance of Identifying Alternative Solutions
To overcome connectivity challenges in rural areas, it is essential to explore low-tech solutions that can bridge the gap in telehealthcare provision and enable access to telehealth services. These telehealth services alternatives can ensure that patients in remote communities receive the necessary support and medical attention despite the limitations posed by poor connectivity options.
Collaboration between telehealthcare providers, technology companies, and government agencies is crucial in effectively addressing the healthcare needs of remote communities and rural areas. By working together, they can develop innovative strategies that enable telehealthcare consultations even in remote communities with limited internet connectivity.
Collaboration between Healthcare Providers, Technology Companies, and Government Agencies
Healthcare providers must collaborate with technology companies specializing in telehealth solutions and remote presence technology to improve access to healthcare in rural areas. By partnering with telehealthcare organizations, they can leverage their expertise to develop customized systems that cater specifically to the needs of rural care settings.
Government agencies also play a vital role in facilitating improved connectivity options for telehealthcare consultations. This is especially important for remote care in rural areas. They can invest in expanding internet infrastructure coverage to reach underserved rural communities, thereby improving access to telehealthcare and remote care services. Governments can provide financial support or incentives for rural healthcare providers who adopt telehealthcare technologies as part of their care system.
Addressing Disparities through Low-Tech Solutions
Low-tech solutions such as using mobile applications or SMS-based platforms can be effective ways to deliver telehealthcare services in rural areas without relying heavily on stable internet connections. These telehealthcare methods allow rural caregivers or patients to communicate with healthcare professionals through text messages or voice calls when accessing video consultations is not feasible.
In rural areas where telehealthcare, including cardiac rehab or other specialized care services, may be limited, telemedicine can provide a possible solution. Remote monitoring devices can be used in rural areas for telehealthcare to track vital signs and transmit data to healthcare professionals for analysis and guidance. This enables rural patients to receive the necessary telehealthcare and support even from a distance, et al.
Low-Tech Solutions for Telemedicine Connectivity
Exploration of low-tech alternatives
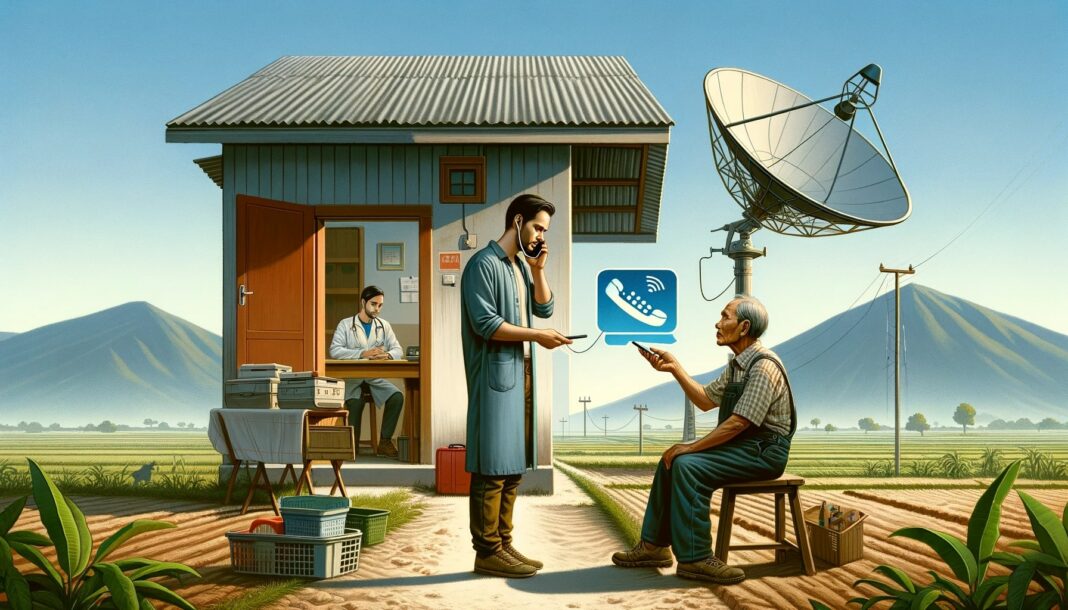
In rural areas where access to reliable internet connectivity is limited, healthcare providers are exploring low-tech alternatives to ensure seamless telehealthcare services. One such alternative for rural health care is the use of satellite-based internet connections for remote care and telehealthcare. By leveraging satellite technology, healthcare professionals can establish a stable and consistent internet connection for telehealthcare, overcoming the challenges posed by traditional broadband infrastructure limitations in rural areas.
Another low-tech alternative that has gained traction is utilizing mobile networks for telehealthcare and remote care, especially in rural areas with limited access to health care. Mobile devices, such as smartphones and tablets, can be used for telehealthcare to connect with patients in rural areas and provide remote health care. These telehealthcare devices can leverage existing mobile network coverage to facilitate remote care consultations and transmit vital health information, especially in rural areas.
Utilization of offline storage devices and portable diagnostic tools
Intermittent connectivity poses a significant challenge in remote areas. To address the issue of limited or no internet access in rural areas, healthcare providers are turning to telehealthcare and utilizing offline storage devices and portable diagnostic tools. Offline storage devices enable healthcare professionals in rural areas to store patient data locally on their devices and synchronize it with the central telehealthcare system once connectivity is restored.
Portable diagnostic tools play a crucial role in providing accurate assessments for remote care, telehealthcare, and rural health care, even when there is no real-time connection available. These telehealthcare tools enable doctors to capture essential health care data, such as blood pressure readings or ECG results, for remote care. The data can be stored locally and later shared with specialists for analysis, particularly benefiting rural areas.
Integration of text messaging and phone calls as backup communication methods
When faced with limited or unreliable internet access in rural areas, telehealthcare practitioners are integrating text messaging and phone calls as backup communication methods for remote care in the health care industry. Text messaging in telehealthcare enables quick information exchange between healthcare providers and rural patients without relying on an active internet connection. Similarly, phone calls provide an effective means of communication when video consultations are not feasible due to technical limitations in telehealth and remote care for rural health care.
By incorporating these backup communication options into their telehealth solutions, healthcare providers can ensure continuous care delivery even in areas where internet connectivity may be sporadic or unavailable for extended periods.
Overcoming equipment malfunctions with low-tech solutions
Technical support and maintenance of telehealth technology can be challenging in remote areas. In the event of remote care equipment malfunctions, low-tech solutions can help bridge the gap until telehealth repairs or replacements are possible in the health care industry. For instance, telehealth healthcare providers can have backup systems or alternative equipment readily available to minimize disruptions in patient care.
Having contingency plans in place and training healthcare professionals on troubleshooting common telehealth issues can further mitigate the impact of equipment failures. This proactive approach ensures that patients continue to receive quality telehealth care despite technical challenges.
Case Studies: Successful Telemedicine Implementation in Rural Areas
Examples showcasing how telemedicine has been effectively utilized in remote regions around the world
Telehealth, also known as telemedicine, has proven to be a game-changer for rural patients, bringing healthcare services closer to their doorstep. Numerous examples from different parts of the globe highlight the successful implementation of telehealth in remote areas, et al. These telehealth case studies demonstrate how technology can bridge the gap and improve access to quality healthcare for rural communities.
One such example is the Pulmonary Rehabilitation Program, a form of telehealth and remote care, implemented in rural Australia to provide accessible health care. This telehealth program aimed to provide specialized care for patients suffering from chronic lung diseases. By utilizing telehealth, patients were able to receive remote care with respiratory specialists without traveling long distances to urban areas. The telehealth program included remote care video consultations, educational resources, and personalized exercise plans tailored to each patient’s health care needs. As a result of telehealth, rural residents gained access to specialized care that was previously limited only to urban areas.
Highlighting specific projects that have overcome connectivity challenges using innovative approaches
In addition to addressing connectivity challenges, some telehealth projects have gone above and beyond by adopting innovative approaches to ensure seamless telemedicine services in remote regions. These projects have revolutionized health care delivery in underserved areas. One notable example is the Health Care Lifestyle Change Program implemented in a rural community in the United States, utilizing telehealth and remote care. This program focused on promoting healthy lifestyle changes among individuals at risk of developing chronic diseases like diabetes and heart disease through telehealth and remote care.
To overcome connectivity challenges faced by this community, they introduced a hybrid model that combined both telehealth and remote care components in addition to traditional health care. Participants received educational materials through mail or local community centers while also engaging in virtual group sessions facilitated by healthcare professionals via telehealth video conferencing platforms. This unique telehealth approach allowed participants from even the most remote areas with limited internet access to benefit from the program.
Demonstrating positive outcomes achieved through improved access to healthcare services via telemedicine
The implementation of telehealth and remote care programs in rural areas has yielded numerous positive outcomes for both patients and communities alike. By improving access to healthcare services through telehealth, telemedicine has enhanced the overall well-being of rural residents.
For instance, telehealth-based disease management programs, including remote care, have shown significant improvements in chronic disease control and prevention, et al. Patients with conditions such as diabetes, hypertension, and asthma have experienced better management of their health through regular telehealth consultations with healthcare providers. This has resulted in reduced hospitalizations and improved medication adherence for rural patients through telehealth and remote care, leading to better overall health outcomes.
Moreover, telehealth, also known as remote care or telemedicine, has played a crucial role in emergency situations where timely access to medical expertise can be life-saving. Remote communities without immediate access to emergency care facilities have benefited from telemedicine-enabled consultations with specialists, using telehealth, who can guide local healthcare providers in delivering appropriate treatment.
Financial Considerations for Telehealth in Remote Locations
Implementing and maintaining telehealth infrastructure in remote areas comes with its fair share of cost implications. However, the potential cost savings and benefits of telehealth and remote care make it a worthwhile investment.
Cost Implications
The initial setup and ongoing maintenance of remote care telehealth facilities can be costly. There are several factors to consider when evaluating the financial impact of telehealth and remote care.
-
Facilities: Building or retrofitting facilities to accommodate telehealth equipment and provide a conducive environment for remote care virtual consultations.
-
Reimbursement: Ensuring that healthcare providers are adequately reimbursed for telehealth visits, as reimbursement rates may vary.
-
Staffing: Hiring and training additional staff members who are proficient in telehealth and remote care technology, ensuring smooth operations and patient satisfaction.
-
Equipment and Technology: Investing in telehealth hardware, software, and connectivity solutions to facilitate seamless remote care virtual consultations.
Potential Cost Savings
While there are upfront costs associated with implementing telehealth in remote areas, there are also significant potential cost savings over time:
-
Reduced Hospital Visits: Telehealth allows patients to receive care remotely without having to travel long distances or visit hospitals unnecessarily. This can lead to reduced hospital admissions, emergency room visits, outpatient appointments, and telehealth.
-
In rural areas where specialized medical services may be limited, telehealth can enable healthcare providers to consult with specialists remotely, avoiding unnecessary transfers. This reduces the need for costly transfers to urban centers for specialized care, making telehealth a more affordable and convenient option.
-
Efficient Chronic Disease Management: Telehealth offers an opportunity for proactive management of chronic conditions through regular remote monitoring and follow-up visits. By utilizing telehealth to prevent complications or exacerbations that require hospitalization, significant cost savings can be achieved.
Funding Sources
To support telehealth initiatives targeting underserved rural communities, various funding sources or grants are available:
-
Federal Programs: The Federal Communications Commission (FCC) offers funding through programs such as the Rural Health Care Program’s Telecommunications Program and the COVID-19 Telehealth Program.
-
State and Local Initiatives: Many states have established grant programs to support telehealth expansion in rural areas. These telehealth programs aim to bridge the digital divide and improve access to telehealthcare services.
-
Nonprofit Organizations: Several nonprofit organizations provide grants and resources specifically for telehealth projects in remote areas. For example, the Rural Health Resource Center offers funding opportunities and technical assistance for telehealth.
By leveraging these funding sources, healthcare providers can alleviate some of the financial concerns associated with implementing telehealth in remote locations.
Ensuring Data Privacy and Rights in Telemedicine
Protecting patient data privacy is of utmost importance in telehealth consultations, especially in remote areas where connectivity challenges may pose additional risks to telehealth services. The legal and ethical considerations surrounding telehealth data security must be carefully addressed to ensure the confidentiality and integrity of sensitive health information.
One key aspect of safeguarding patient privacy in telehealth is the implementation of robust encryption protocols. By encrypting data during transmission and storage, telehealth providers can prevent unauthorized access or interception by third parties. This ensures that patient information remains secure throughout the telehealth consultation process.
Adherence to telehealth privacy regulations is another crucial factor in maintaining data privacy in remote healthcare settings. Telehealth providers must comply with relevant laws such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States or similar regulations in other countries. These telehealth regulations outline specific requirements for protecting patient health information and impose penalties for non-compliance.
In addition to encryption and regulatory compliance, there are several best practices that can help ensure data privacy during telemedical consultations with telehealth.
Consent and Authorization
Obtaining informed consent from patients before engaging in telehealth consultations is essential for telemedicine. Patients should be fully aware of how their health information will be collected, used, stored, and shared during the telehealth encounter.
Secure Technology Infrastructure
Telehealth platforms should have robust security measures in place to protect against unauthorized access. This includes implementing firewalls for telehealth, regularly updating telehealth software systems, using secure servers for storing telehealth patient data, and employing multi-factor authentication for telehealth user access.
Training and Education
Healthcare professionals involved in telemedicine should receive proper training on telehealth data privacy practices. They should understand how to handle sensitive information securely in the context of telehealth, including telehealth password management, recognizing telehealth phishing attempts, and following appropriate protocols for sharing patient records in the telehealth setting.
Data Retention Policies
Establishing clear guidelines on how long patient data will be retained in telehealth is crucial for maintaining privacy. Telehealth providers should develop policies that outline the duration for which data will be stored and establish protocols for secure deletion or disposal of information once it is no longer needed.
Transparency and Patient Rights
Telehealth providers should clearly communicate their privacy practices to patients, including how their data will be used, shared, and protected. Patients should also have the right to access their telehealth information and request corrections or updates to ensure accuracy.
While telemedicine, also known as telehealth, offers numerous benefits in terms of accessibility and convenience, it is essential to prioritize patient privacy throughout the telehealth process. By implementing robust encryption protocols, adhering to privacy regulations, obtaining informed consent, maintaining a secure technology infrastructure, providing training on data privacy practices, establishing data retention policies, and ensuring transparency and patient rights, telehealth providers can overcome connectivity challenges in remote areas while safeguarding patient confidentiality.
Overcoming Connectivity Challenges in Telemedicine
We have also delved into low-tech solutions for overcoming connectivity issues and shared case studies showcasing successful telehealth implementation in rural locations. We have touched upon the financial considerations and the importance of ensuring data privacy and rights in telehealth.
Moving forward, it is crucial for healthcare providers, policymakers, and technology developers to collaborate closely to bridge the connectivity gap in remote areas and promote telehealth. By investing in infrastructure development, such as expanding broadband networks and improving cellular coverage, we can enhance telehealth capabilities even further. Furthermore, exploring innovative low-tech solutions like offline storage devices or satellite-based communication systems can provide reliable connectivity options for telehealth where traditional internet access is limited.
By adopting these measures, we can empower healthcare professionals to reach patients in remote areas seamlessly through telehealth. It is essential that stakeholders prioritize telehealth efforts to ensure equitable access to quality telehealthcare services regardless of geographical location. Together, let us strive towards a future where telehealth and telemedicine become vital tools for improving healthcare outcomes in even the most underserved communities.
FAQs
How does telemedicine benefit patients in remote areas?
Telehealth, also known as telemedicine, offers numerous benefits for patients residing in remote areas, et al. Telehealth allows individuals to receive timely medical consultations without the need to travel long distances or face transportation challenges. Through telehealth, patients can connect with healthcare professionals from the comfort of their homes while still receiving quality care via virtual appointments. Telemedicine, or telehealth, also enables specialists located elsewhere to provide expertise remotely, expanding access to specialized care that may not be readily available locally.
What are some low-tech solutions for overcoming connectivity challenges?
In regions with limited internet connectivity, several low-tech solutions can help overcome connectivity challenges in telehealth. One example of utilizing telehealth is using offline storage devices that allow patient data to be collected during periods of no or intermittent connection and then uploaded once an internet connection is available. Another option for reliable connectivity, especially in remote areas where traditional internet access may be scarce, is leveraging satellite-based communication systems. This can be particularly beneficial for telehealth services.
How can telemedicine implementation be financially feasible in remote locations?
Telehealth implementation in remote areas can be financially feasible through various telemedicine strategies. One approach is to secure funding from government grants or healthcare organizations specifically designated for expanding telehealth services in underserved communities. Forming partnerships with local healthcare providers and community organizations can help share costs and resources, making telehealth more economically viable. It is also important to consider the potential cost savings associated with telehealth, including reduced travel expenses for patients and providers alike.
What measures are taken to ensure data privacy and rights in telemedicine?
Data privacy and rights are paramount in telemedicine. Healthcare providers must adhere to strict security protocols for telehealth to safeguard patient information during virtual consultations, ensuring compliance with relevant regulations such as HIPAA. Secure encryption methods should be employed for telehealth data transmission, while robust authentication processes protect against unauthorized access. Patients should also be educated about their rights concerning their personal health information and how it will be handled during telemedicine interactions.
Can telemedicine completely replace in-person medical visits?
While telemedicine offers numerous advantages, it cannot entirely replace in-person medical visits. Some conditions require physical examinations or procedures that cannot be conducted remotely. However, telemedicine serves as a valuable complement to traditional healthcare by providing convenient access to routine check-ups, follow-up appointments, mental health support, and chronic disease management. It enhances healthcare accessibility while still recognizing the importance of face-to-face interactions when necessary for comprehensive care delivery.