What might healthcare look like ten years from now? It’s a question a lot of people are asking. The last decade brought us some vital discoveries and medical advances, some of which have revolutionized disease treatment and set the stage for future research. These discoveries have opened up possibilities that only a decade ago were mere imaginations.
Take cancer research and treatment, for example. Michael Teitell, PhD., Managing Director of UCLA Johnson Comprehensive Cancer Center, says that 15 to 20 years ago, immunotherapies for cancer were a wild dream.
“Cancer was considered a death sentence back then,” the medical doctor says. “But now, immune checkpoint inhibitors and adoptive immune cell therapies are creating hope, with preliminary trials showing huge promise.”
Cardiology is another area where tremendous progress was made in the last decade. Speaking to UCLA health last year, Gregg Fonarow, MD, the Eliot Corday Chair in Cardiovascular Medicine, says one of the most important advances in cardiovascular disease treatment is the development of the TAVR – happened within the last decade.
“It is one of the most important advancements in cardiology,” he says of the development of the transcatheter aortic valve replacement (TAVR) technology. “It provides us with a simpler, safer implantation strategy and has allowed us to reach a broader population of patients.”
The two above are just examples of the tremendous progress made in healthcare in the last decade. There were many other advancements in several other areas. In the field of HIV/AIDS, for instance, we saw the development of Pre-Exposure Prophylaxis (PrEP) pills that when taken once daily, prevents HIV infection in at-risk populations.
Multiple Sclerosis (MS), Alzheimer’s, sleep, and nutrition are the other areas where healthcare treatment made significant progress.
Could we witness similar advancements between 2020 and 2030? And, if so, what developments are we likely to see?
Healthcare Advancements to Look Forward to in the Next Decade
Dimensional Insight outlines four key factors that will drive healthcare discoveries and innovations in the next decade, i.e., measuring patient success through feedback, serving marginalized societies, and better assessing the societal determinants of health.
With these factors in mind, some of the biggest healthcare advancements that could define the next decade are;
1. Further progress in care for Alzheimer’s
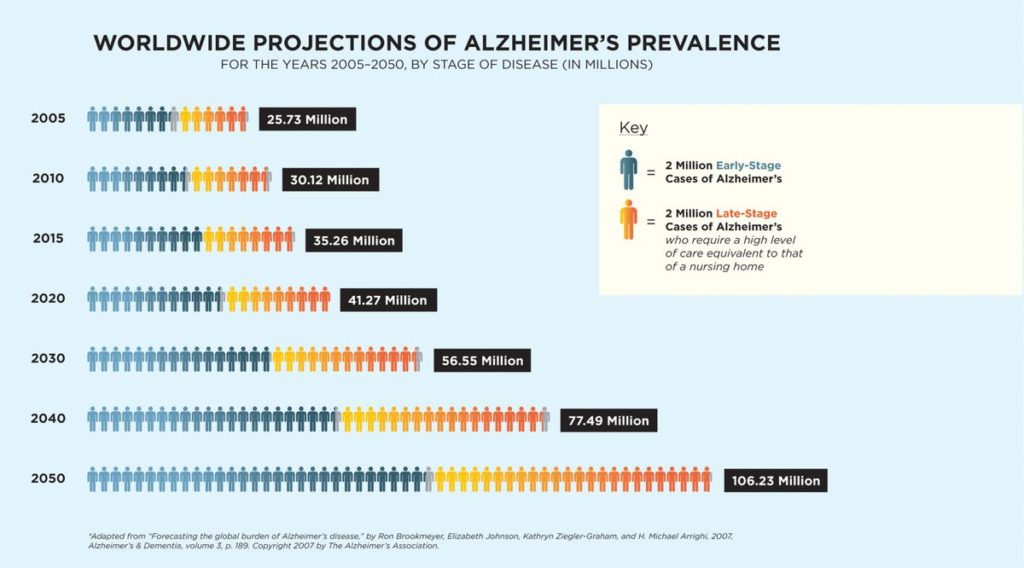
Alzheimer’s, which is the primary cause of dementia, affects tens of millions globally. In the US, the disease affects 5.8 million people and is the sixth-leading cause of death, according to the Alzheimer’s Association. This population (of Alzheimer’s patients) is expected to reach 14 million by 2050, a scary statistic, to say the least.
Current treatments temporarily improve symptoms of memory loss and issues related to thinking and sensing. The treatments do so by boosting the performance of brain cells that carry information from one brain cell to another. Unfortunately, none of these treatments stop the underlying decline and death of brain cells, which is the primary cause of Alzheimer’s.
Experts predict that the next decade could present us with new medications and treatments that stop or delay Alzheimer’s progression. One treatment approach currently under research, for instance, takes aim at plaques i.e., the microscopic clumps of the protein beta-amyloid, a characteristic feature of Alzheimer’s.
Another treatment approach currently under research involves keeping tau from tangling. A vital brain cell transport system is compromised when a protein called tau twists to form tangles (microscopic fibers). The result is a brain anomaly that exuberates Alzheimer’s symptoms. Researchers are currently looking for ways to prevent the tangling. Indeed, there are already a few tau vaccines and aggregation inhibitors in the pipeline.
Finally, there’s ongoing research on ways to minimize or slow down the chronic low-level brain cell inflammation, which is another hallmark of Alzheimer’s. There’s also ongoing work in areas of insulin resistance. In all these areas, researchers see very positive results, which gives hope that we could see a lot of progress in Alzheimer’s treatment by the end of the decade.
2. Progress in cancer treatment/management
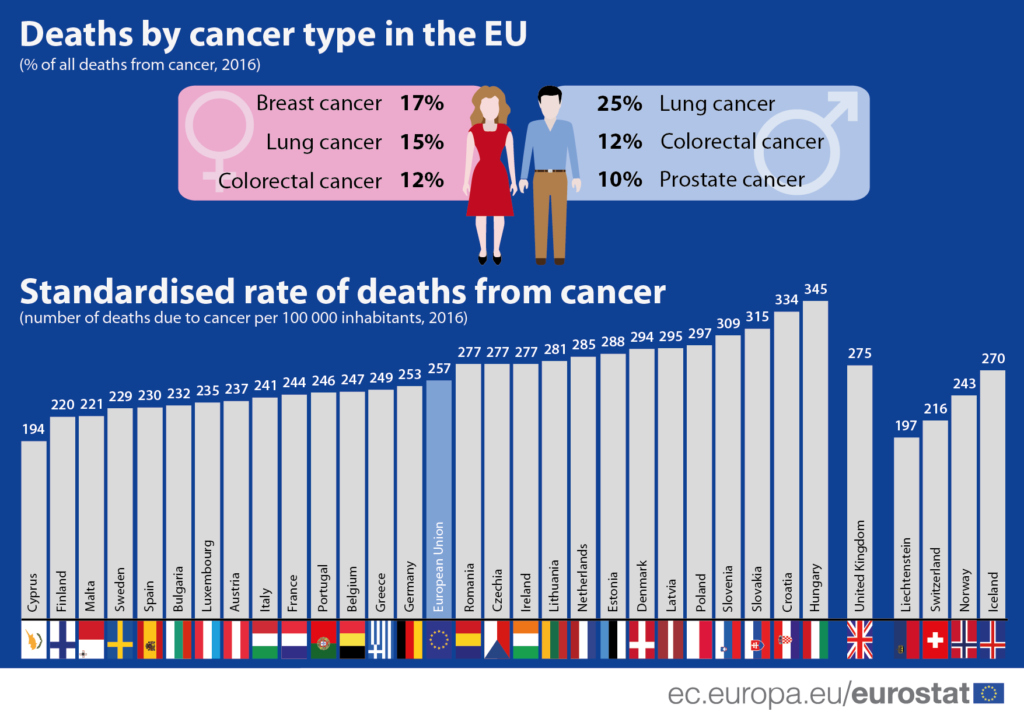
An estimated 18 million people are living with cancer worldwide. Lung (12.3%) and breast (12.3%) are the most common cancer types, with colorectal (10.6%), prostate (7.5%), and stomach (6.1%) cancers following in that order.
Thankfully, tremendous progress was made in cancer research and treatment in the last decade. Precision treatment was one such advancement that has had a massive impact on cancer management and treatment. Precision treatment allows doctors to identify and utilize only therapies that are most likely to be successful in treating an individual’s cancer based on detailed genetic information. We’ve also seen some progress in the development of cancer vaccines.
Research is ongoing in all these areas, especially precision treatment. However, for the next decade, the biggest breakthroughs are expected in gene therapy
Gene therapy is a way of treating or preventing disease by altering the genetic instructions within an individual’s cells. Genes are responsible for pretty much every aspect of the cell’s life. They determine how and when the cells grow, how they function, and even when they divide or die. Gene therapy attempts to solve two main challenges – hyperactive genes and missing genes. In cancer treatment, it also helps in expressing entirely foreign genes in cells to alter their function or survival.
One gene therapy approach, CAR T-cell therapy, has received approval from the FDA for use in certain patients. CAR T-cell therapy, a form of immunotherapy, helps the immune system find and kill cancer tumors. Expect significant progress in CAR T-cell therapy and gene therapy in general over the next decade.
3. Hepatitis C treatment
Caused by the hepatitis C virus (HCV), hepatitis C was only discovered a few decades ago but is currently one of the biggest health challenges worldwide. It causes an acute infection, which may lead to chronic infection in up to 85% of the patients. The virus carries many life-threatening risks, including hepatocellular carcinoma (HCC) and end-stage live disease (ESLD). Currently, 185 million people live with Hepatitis C globally.
The two biggest problems with HCV treatment are lack of awareness and costly medication. For a disease that currently affects about 3% of the global population, it’s staggering that more than half of Hepatitis C patients don’t know they have the virus. Additionally, although present HCV treatments work, it’s been shown that they are only effective in half of the patients. The drugs have unwanted side effects that make it difficult or impossible for some patients to use them.
Progress is being made on both fronts. First off, there’s research aimed at developing more accurate diagnostic tests. Although current tests detect HCV, they are expensive and not 100% effective. In many cases, the tests fail to detect infections (false negatives).
These two issues have significantly contributed to the high number of people living with HCV without being aware that they have the disease. Researches are working on developing less expensive and more reliable tests.
Concerning medications, just recently, the FDA approved a new two-drug combo, Harvoni, which can cure Hepatitis C in just eight weeks. Harvoni also comes with fewer and less severe side effects. The only downside is that the drug is costly. It’s also worth noting that efforts are underway to develop a vaccine for Hepatitis C.
4. Customized medication (genomics)
Genomics, or precision medicine, is arguably the most exciting area in medicine right now. A novel approach to disease treatment and cure, genomics relies on genetic information, environmental conditions, and patient lifestyle to determine the best treatment option for the individual patient.
Don’t confuse it with personalized medicine. While personalized medicine also incorporates the genetic makeup of the individual and their social and religious interests, genomics relies heavily on data and analytics to find the ultimate patient-centered course of treatment. Precision medicine can, therefore, be thought of as a more customized subset of personal medicine.
The first successful application of precision medicine was in 2010 when doctors used genetic sequencing to treat Alexis and Noah Beery of the cerebral palsy. After an earlier misdiagnosis. However, the applications have increased recently, with prenatal screening tests perhaps the biggest evidence of where genomics could take us. The now widely available screening tests allow doctors to draw fragments of placental DNA from maternal blood to determine genetic abnormalities.
In the next decade, experts see genome sequencing playing a role in two key areas; as a noninvasive screening test for preventing medicine and as a test to improve diagnostic capabilities.
Early data indicates that gene sequencing would lead to valuable insight into future disease risks, with oncology and psychiatry two of the fields likely to benefit the most. With the help of Big Data, there should be enough information to reference sequences, identify individualized patient factors, and map phonetic expressions. The Global Alliance for Genomics and Health (GA4GH) predicts that 60 million genomes will be collected by 2025 to create a multifactor database where individually sequenced can be compared.
5. The era of smart antibiotics and antibiotic programs
In 2016, a woman in Nevada died of an infection that resisted every antibiotic available to doctors in the US, including carbapenems, considered a last line of defense against infectious diseases. That’s when the “superbug” became a reality – a bug that isn’t treatable with standard antibiotics. While infections of this type are still rare, it was a wake-up call for everyone, and not just in healthcare.
What’s the solution? Smarter drugs. You see, microbes are incredibly adaptive. They don’t change their habits quickly. But, over time, which can be decades or even an entire generation, they will find a way to mutate to threats in their environment. Currently, antibiotics form the biggest threat to microbes, and it looks like they’re already adapting.
What further complicates the problem is the difficulty of controlling superbugs. According to Dr. Mathew J. Bankowski, Ph.D., MS, and Clinical and Molecular Microbiology Laboratory Director at Baptist Medical Center in Florida, it can result in “untreatable bugs.”
A few experts foresee a future where smart antibiotics will be developed that only deploy if a bacterial pathogen causing the infection being treated is present. These smart antibiotics would also comprise multiple strains and work in such a way that only the necessary strain is activated while the other strains remain dormant. This should help prevent bacterial resistance.
Another approach, and a solution you’ll likely see sooner, is antibiograms that keep records of resistant bacteria to help doctors select treatments that are more likely to be effective.
6. 3D drug printing goes mainstream
Last year (2019) marked a major milestone in the pharmaceutical industry when the FDA approved Aprecia Pharmaceuticals’ Spritam (levetiracetam) tablets. The drugs are manufactured using 3D technology. An inkjet printing process produces the porous water-soluble drug layer by layer without compression or traditional molding techniques.
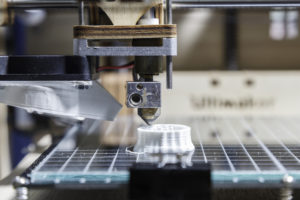
It’s a fascinating area, according to most healthcare experts, and a topic to keep an eye on. “To date, 3D printing has been all about printing plastic and metal parts, especially for the manufacturing industry,” says Laura Dormer, Editorial Director for Future Medicine. “3D printing in pharmaceuticals isn’t as advanced yet, but offer an exciting opportunity for the future.”
The key driver for 3D printing in pharma is personalized medicine. The conventional drug manufacturing process uses approaches best suited to mass manufacturing. When it comes to personalized medicine where drugs are to be manufactured with the individual’s needs (e.g., shape, size, appearance, etc.) in mind, these methods would be overwhelmed.
“The technology can be used to develop specific drugs or drug cocktails based on an individual,” says Reenita Das, Transformational Health Partner and Senior VP at Frost & Sullivan. “We’re at a stage in healthcare where one-size-fits-all is not ideal. 3D printing allows for mass customization at scale.”
Currently, it might be too early to consider 3D drug printing as an alternative to mass manufacture of drugs, but expect plenty of progress over the next decade. “We’re just scratching the surface,” says Ms. Das. “We will see significant disruption in 5 to 10 years.”
7. The advent of medical tricorders
If you’re hearing about it for the first time, a medical tricorder is a hand-held scanning device that allows consumers to self-diagnose their medical conditions within a fraction of a second. The tricorder can perform the diagnosis as a stand-alone device or with the help of a medical database accessible via the internet.
The first working prototype of a medical tricorder was developed in 2017 by Philadelphia-based emergency room physician Basil Harris, and made available at $200. “It does exactly what I do in the ER,” Harris explained during the 2017 Qualcomm Tricorder XPRIZE competition. “It starts by monitoring the patient’s vitals then proceeds to ask questions to understand the symptoms before giving a diagnosis.”
It’s been three years now, and it looks like even more people have jumped on the bandwagon, with Apple and Accenture becoming some of the top funders of tricorder devices. According to Market research Future, the global market for medical tricorders is set to reach $5.4 billion, with a CAGR of approximately 6.7%.
However, it’s important to note that these devices will eventually need to pass regulatory standards, which could increase approval time. The average approval time for devices of this nature is 5-8 years. It means that it could be 2022 at the earliest before we see the first FDA-approved medical tricorder.
Nevertheless, expect to see a few such devices come to the market (even before FDA approval). The Vitaliti from Cloud DX, for instance, is scheduled to enter the market between 2020 and 2021. Vitaliti is capable of continuously measuring all of a patient’s vitals and analyzing tiny samples of bodily fluids to diagnose 19 separate medical conditions autonomously.
8. The robots finally arrive
Robots aren’t a new phenomenon, even in the healthcare industry. We’re currently accustomed to chatting with care providers using AI chatbots. Though they’re the most basic form of artificial intelligence, chatbots are robots nonetheless.
Robotic medical assistants are also widely used to monitor patient vitals and alert nurses when there’s a need for human intervention. Some robots also help healthcare personnel automatically enter information into patient electronic health records. These are now standard in many modern hospitals where they save valuable time and boost accuracy.
Recent advancements in the field mean that we’ll only see more of these robots in healthcare – only smarter and more intelligent. One such development is the robotic lab assistant, predicted to come to the market in a few years. A robotic lab assistant can locate blood vessels and draw blood with less pain and anxiety. It can also prepare and dispense medications in labs.
Another advanced robot expected in healthcare soon is the telenursing robot. A telenursing robot remains physically accessible to the patient and features a user interface from which the nurse or healthcare provider operates it. These robots’ functions include intaking consultations/patient rounds, turning off alarms, moving equipment carts, supplying food and meds, and feeding patients by mouth.
An example of a telenursing robot project currently underway is TRINA. The TRINA project intends to create a robot named TRINA, which should be available in a few years.
Summary
Healthcare is changing. Spurred by advances in technology and research, we’re entering a new age in medicine where some of the perennial problems we’ve had for the past generation could finally be resolved. These include diseases such as cancer and Alzheimer’s, as well as antibiotic resistance and achieving personalized care.
As long as research on these eight areas is sustained, it’s only a matter of time before we see revolutionary breakthroughs. It’s likely that many of those breakthroughs will come in this decade.
Contact Nix Solutions to learn more about emerging technologies and discover ways to grow your practice or business.



